Search
- Page Path
- HOME > Search
- Thyroid
- Prognostic Roles of Inflammatory Biomarkers in Radioiodine-Refractory Thyroid Cancer Treated with Lenvatinib
- Chae A Kim, Mijin Kim, Meihua Jin, Hee Kyung Kim, Min Ji Jeon, Dong Jun Lim, Bo Hyun Kim, Ho-Cheol Kang, Won Bae Kim, Dong Yeob Shin, Won Gu Kim
- Endocrinol Metab. 2024;39(2):334-343. Published online April 4, 2024
- DOI: https://doi.org/10.3803/EnM.2023.1854
- 340 View
- 24 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
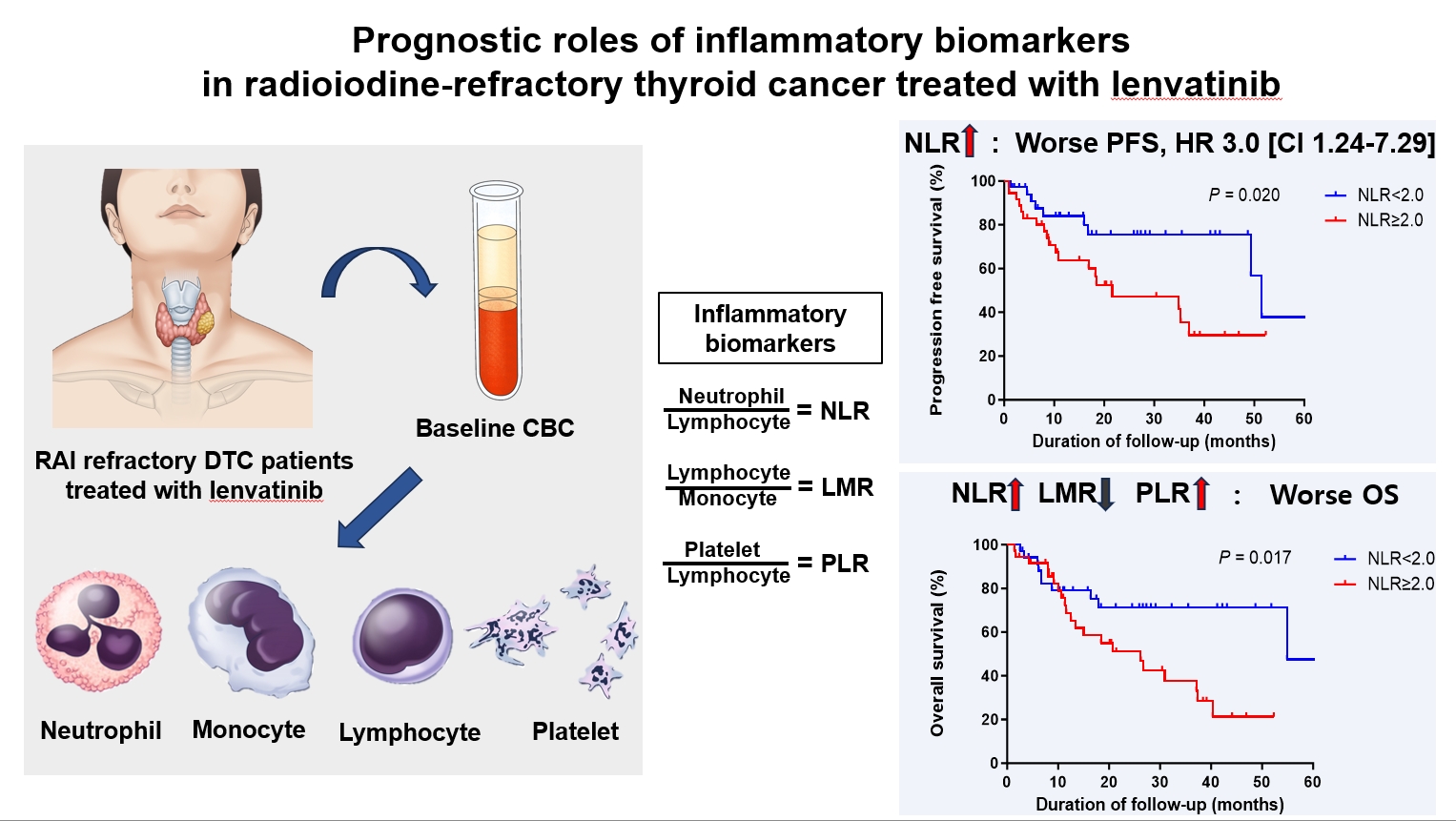
ePub - Background
Inflammatory biomarkers, such as the neutrophil-to-lymphocyte ratio (NLR), lymphocyte-to-monocyte ratio (LMR), and platelet-to-lymphocyte ratio (PLR), serve as valuable prognostic indicators in various cancers. This multicenter, retrospective cohort study assessed the treatment outcomes of lenvatinib in 71 patients with radioactive iodine (RAI)-refractory thyroid cancer, considering the baseline inflammatory biomarkers.
Methods
This study retrospectively included patients from five tertiary hospitals in Korea whose complete blood counts were available before lenvatinib treatment. Progression-free survival (PFS) and overall survival (OS) were evaluated based on the median value of inflammatory biomarkers.
Results
No significant differences in baseline characteristics were observed among patients grouped according to the inflammatory biomarkers, except for older patients with a higher-than-median NLR (≥2) compared to their counterparts with a lower NLR (P= 0.01). Patients with a higher-than-median NLR had significantly shorter PFS (P=0.02) and OS (P=0.017) than those with a lower NLR. In multivariate analysis, a higher-than-median NLR was significantly associated with poor OS (hazard ratio, 3.0; 95% confidence interval, 1.24 to 7.29; P=0.015). However, neither the LMR nor the PLR was associated with PFS. A higher-than-median LMR (≥3.9) was significantly associated with prolonged OS compared to a lower LMR (P=0.036). In contrast, a higher-than-median PLR (≥142.1) was associated with shorter OS compared to a lower PLR (P=0.039).
Conclusion
Baseline inflammatory biomarkers can serve as predictive indicators of PFS and OS in patients with RAI-refractory thyroid cancer treated with lenvatinib.

- Miscellaneous
- Corrigendum: Correction of Acknowledgments. Protocol for a Korean Multicenter Prospective Cohort Study of Active Surveillance or Surgery (KoMPASS) in Papillary Thyroid Microcarcinoma
- Min Ji Jeon, Yea Eun Kang, Jae Hoon Moon, Dong Jun Lim, Chang Yoon Lee, Yong Sang Lee, Sun Wook Kim, Min-Hee Kim, Bo Hyun Kim, Ho-Cheol Kang, Minho Shong, Sun Wook Cho, Won Bae Kim
- Endocrinol Metab. 2022;37(1):181-182. Published online February 28, 2022
- DOI: https://doi.org/10.3803/EnM.2022.104
- Corrects: Endocrinol Metab 2021;36(2):359
- 2,803 View
- 110 Download
- 1 Web of Science
- 1 Crossref
-
 PDF
PDF PubReader
PubReader  ePub
ePub -
Citations
Citations to this article as recorded by- Risk of thyroid cancer associated with glucagon‐like peptide‐1 receptor agonists and dipeptidyl peptidase‐4 inhibitors in patients with type 2 diabetes: A population‐based cohort study
Sungho Bea, Heejun Son, Jae Hyun Bae, Sun Wook Cho, Ju‐Young Shin, Young Min Cho
Diabetes, Obesity and Metabolism.2024; 26(1): 108. CrossRef
- Risk of thyroid cancer associated with glucagon‐like peptide‐1 receptor agonists and dipeptidyl peptidase‐4 inhibitors in patients with type 2 diabetes: A population‐based cohort study

- Thyroid
- Clinical Characteristics and Prognosis of Coexisting Thyroid Cancer in Patients with Graves’ Disease: A Retrospective Multicenter Study
- Jee Hee Yoon, Meihua Jin, Mijin Kim, A Ram Hong, Hee Kyung Kim, Bo Hyun Kim, Won Bae Kim, Young Kee Shong, Min Ji Jeon, Ho-Cheol Kang
- Endocrinol Metab. 2021;36(6):1268-1276. Published online November 26, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1227
- 4,837 View
- 186 Download
- 10 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
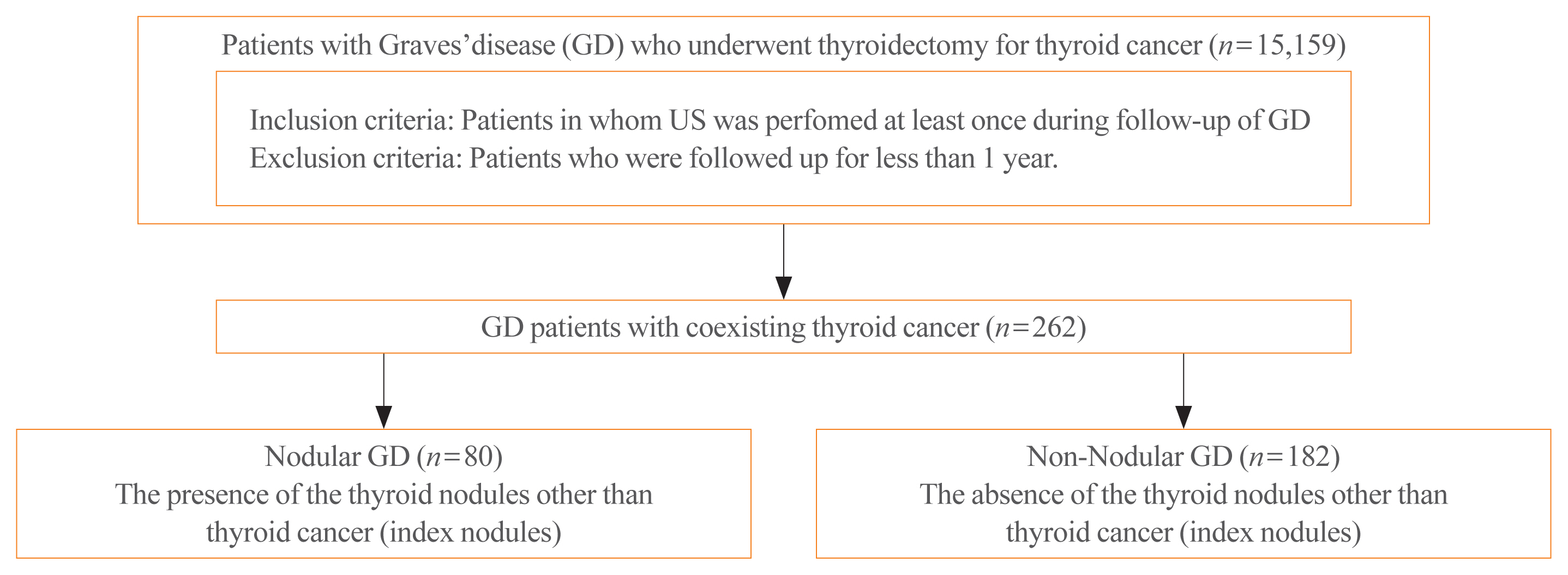
The association between Graves’ disease (GD) and co-existing thyroid cancer is still controversial and most of the previously reported data have been based on surgically treated GD patients. This study investigated the clinicopathological findings and prognosis of concomitant thyroid cancer in GD patients in the era of widespread application of ultrasonography.
Methods
Data of GD patients who underwent thyroidectomy for thyroid cancer between 2010 and 2019 in three tertiary hospitals in South Korea (Asan Medical Center, Chonnam National University Hwasun Hospital, and Pusan National University Hospital) were collected and analyzed retrospectively. In the subgroup analysis, aggressiveness and clinical outcomes of thyroid cancer were compared nodular GD and non-nodular GD groups according to the presence or absence of the thyroid nodules other than thyroid cancer (index nodules).
Results
Of the 15,159 GD patients treated at the hospitals during the study period, 262 (1.7%) underwent thyroidectomy for coexisting thyroid cancer. Eleven patients (4.2%) were diagnosed with occult thyroid cancer and 182 patients (69.5%) had microcarcinomas. No differences in thyroid cancer aggressiveness, ultrasonographic findings, or prognosis were observed between the nodular GD and non-nodular GD groups except the cancer subtype. In the multivariate analysis, only lymph node (LN) metastasis was an independent prognostic factor for recurrent/persistent disease of thyroid cancer arising in GD (P=0.020).
Conclusion
The prevalence of concomitant thyroid cancer in GD patients was considerably lower than in previous reports. The clinical outcomes of thyroid cancer in GD patients were also excellent but, more cautious follow-up is necessary for patients with LN metastasis in the same way as for thyroid cancer in non-GD patients. -
Citations
Citations to this article as recorded by- Comparison of Surgical Outcomes of Transoral Versus Open Thyroidectomy for Graves Disease
Suo-Hsien Wang, Wu-Po Chao, Ta-You Lo, Soh-Ching Ng, Yu-Hsien Chen
Surgical Laparoscopy, Endoscopy & Percutaneous Techniques.2024; 34(2): 150. CrossRef - Outcomes of Surgical Treatment for Graves’ Disease: A Single-Center Experience of 216 Cases
Hanxing Sun, Hui Tong, Xiaohui Shen, Haoji Gao, Jie Kuang, Xi Chen, Qinyu Li, Weihua Qiu, Zhuoran Liu, Jiqi Yan
Journal of Clinical Medicine.2023; 12(4): 1308. CrossRef - Cancer and Mortality Risks of Graves’ Disease in South Korea Based on National Data from 2010 to 2019
Young Ju Choi, Kyungdo Han, Won Kyoung Cho, Min Ho Jung, Byung-Kyu Suh
Clinical Epidemiology.2023; Volume 15: 535. CrossRef - Risk and Prognosis of Thyroid Cancer in Patients with Graves’ Disease: An Umbrella Review
Marco Palella, Francesca Maria Giustolisi, Adriana Modica Fiascaro, Martina Fichera, Antonella Palmieri, Rossella Cannarella, Aldo E. Calogero, Margherita Ferrante, Maria Fiore
Cancers.2023; 15(10): 2724. CrossRef - Characteristics, staging and outcomes of differentiated thyroid cancer in patients with and without Graves’ disease
Chaitra Gopinath, Hanna Crow, Sujata Panthi, Leonidas Bantis, Kenneth D. Burman, Chitra Choudhary
Journal of Clinical & Translational Endocrinology.2023; 33: 100321. CrossRef - Prevalence, Treatment Status, and Comorbidities of Hyperthyroidism in Korea from 2003 to 2018: A Nationwide Population Study
Hwa Young Ahn, Sun Wook Cho, Mi Young Lee, Young Joo Park, Bon Seok Koo, Hang-Seok Chang, Ka Hee Yi
Endocrinology and Metabolism.2023; 38(4): 436. CrossRef - Hashimoto’s Thyroiditis and Papillary Thyroid Carcinoma: A Follow-Up Study in Patients with Absence of Aggressive Risk Factors at the Surgery of the Primary Tumor
Andrea Marongiu, Susanna Nuvoli, Andrea De Vito, Sonia Vargiu, Angela Spanu, Giuseppe Madeddu
Diagnostics.2023; 13(19): 3068. CrossRef - Table of Contents
Clinical Thyroidology.2022; 34(2): 48. CrossRef - Predisposition to and Prognosis of Thyroid Cancer May Not Be Affected by Graves’ Disease, But Some Questions Still Remain
Yanrui Huang, Haixia Guan
Clinical Thyroidology.2022; 34(2): 59. CrossRef - A Comparative Follow-Up Study of Patients with Papillary Thyroid Carcinoma Associated or Not with Graves’ Disease
Andrea Marongiu, Susanna Nuvoli, Andrea De Vito, Maria Rondini, Angela Spanu, Giuseppe Madeddu
Diagnostics.2022; 12(11): 2801. CrossRef - An unusual case of papillary thyroid carcinoma presenting as Graves’ disease
Pooja Tiwari, Uma Kaimal Saikia, Abhamoni Baro, Ashok Krishna Bhuyan
Thyroid Research and Practice.2022; 19(1): 47. CrossRef
- Comparison of Surgical Outcomes of Transoral Versus Open Thyroidectomy for Graves Disease

- Thyroid
- Comparison of Thyroid Imaging Reporting and Data Systems in Malignancy Risk Stratification of Indeterminate Thyroid Nodules
- Bo Hyun Kim
- Endocrinol Metab. 2021;36(5):974-976. Published online October 28, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1287
- 2,794 View
- 102 Download

- Thyroid
- Clinicopathological Characteristics and Disease-Free Survival in Patients with Hürthle Cell Carcinoma: A Multicenter Cohort Study in South Korea
- Meihua Jin, Eun Sook Kim, Bo Hyun Kim, Hee Kyung Kim, Yea Eun Kang, Min Ji Jeon, Tae Yong Kim, Ho-Cheol Kang, Won Bae Kim, Young Kee Shong, Mijin Kim, Won Gu Kim
- Endocrinol Metab. 2021;36(5):1078-1085. Published online October 28, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1151

- 3,883 View
- 110 Download
- 4 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Hürthle cell carcinoma (HCC), a type of thyroid carcinoma, is rare in South Korea, and few studies have investigated its prognosis.
Methods
This long-term multicenter retrospective cohort study evaluated the clinicopathological features and clinical outcomes in patients with HCC who underwent thyroid surgery between 1996 and 2009.
Results
The mean age of the 97 patients included in the study was 50.3 years, and 26.8% were male. The mean size of the primary tumor was 3.2±1.8 cm, and three (3.1%) patients had distant metastasis at initial diagnosis. Ultrasonographic findings were available for 73 patients; the number of nodules with low-, intermediate-, and high suspicion was 28 (38.4%), 27 (37.0%), and 18 (24.7%), respectively, based on the Korean-Thyroid Imaging Reporting and Data System. Preoperatively, follicular neoplasm (FN) or suspicion for FN accounted for 65.2% of the cases according to the Bethesda category, and 13% had malignancy or suspicious for malignancy. During a median follow-up of 8.5 years, eight (8.2%) patients had persistent/recurrent disease, and none died of HCC. Older age, gross extrathyroidal extension (ETE), and widely invasive types of tumors were significantly associated with distant metastasis (all P<0.01). Gross ETE (hazard ratio [HR], 27.7; 95% confidence interval [CI], 2.2 to 346.4; P=0.01) and widely invasive classification (HR, 6.5; 95% CI, 1.1 to 39.4; P=0.04) were independent risk factors for poor disease-free survival (DFS).
Conclusion
The long-term prognosis of HCC is relatively favorable in South Korea from this study, although this is not a nation-wide data, and gross ETE and widely invasive cancer are significant prognostic factors for DFS. The diagnosis of HCC by ultrasonography and cytopathology remains challenging. -
Citations
Citations to this article as recorded by- Molecular Alterations and Comprehensive Clinical Management of Oncocytic Thyroid Carcinoma
Lindsay A. Bischoff, Ian Ganly, Laura Fugazzola, Erin Buczek, William C. Faquin, Bryan R. Haugen, Bryan McIver, Caitlin P. McMullen, Kate Newbold, Daniel J. Rocke, Marika D. Russell, Mabel Ryder, Peter M. Sadow, Eric Sherman, Maisie Shindo, David C. Shonk
JAMA Otolaryngology–Head & Neck Surgery.2024; 150(3): 265. CrossRef - Oncocytic carcinoma of the thyroid: Conclusions from a 20‐year patient cohort
Nelson R. Gruszczynski, Shahzeb S. Hasan, Ana G. Brennan, Julian De La Chapa, Adithya S. Reddy, David N. Martin, Prem P. Batchala, Edward B. Stelow, Eric M. Dowling, Katherine L. Fedder, Jonathan C. Garneau, David C. Shonka
Head & Neck.2024;[Epub] CrossRef - Hurthle cell carcinoma: a rare variant of thyroid malignancy – a case report
Yuvraj Adhikari, Anupama Marasini, Nawaraj Adhikari, Laxman D. Paneru, Binit Upadhaya Regmi, Manita Raut
Annals of Medicine & Surgery.2023; 85(5): 1940. CrossRef - Hürthle Cell Carcinoma: Single Center Analysis and Considerations for Surgical Management Based on the Recent Literature
Costanza Chiapponi, Milan J.M. Hartmann, Matthias Schmidt, Michael Faust, Christiane J. Bruns, Anne M. Schultheis, Hakan Alakus
Frontiers in Endocrinology.2022;[Epub] CrossRef
- Molecular Alterations and Comprehensive Clinical Management of Oncocytic Thyroid Carcinoma

- Thyroid
- Whole-Exome Sequencing in Papillary Microcarcinoma: Potential Early Biomarkers of Lateral Lymph Node Metastasis
- Mijin Kim, Chae Hwa Kwon, Min Hee Jang, Jeong Mi Kim, Eun Heui Kim, Yun Kyung Jeon, Sang Soo Kim, Kyung-Un Choi, In Joo Kim, Meeyoung Park, Bo Hyun Kim
- Endocrinol Metab. 2021;36(5):1086-1094. Published online October 28, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1132
- 3,598 View
- 109 Download
- 4 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
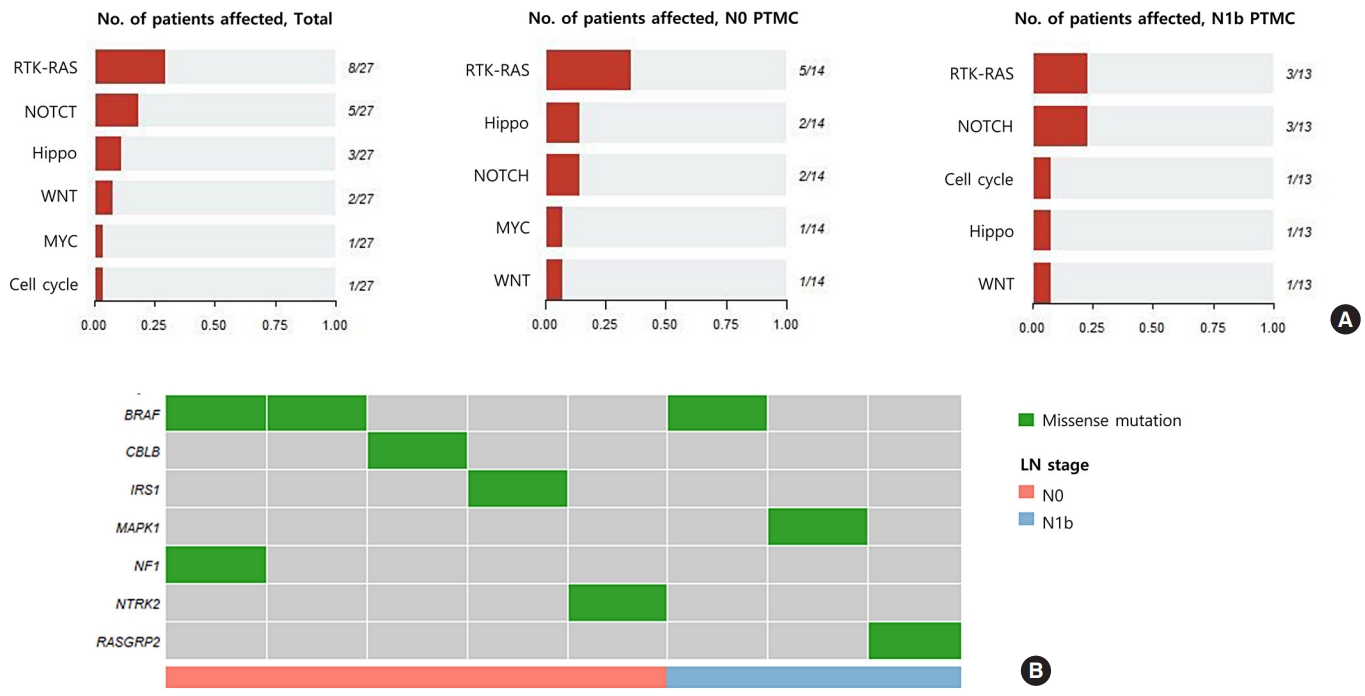
ePub - Background
Early identification of patients with high-risk papillary thyroid microcarcinoma (PTMC) that is likely to progress has become a critical challenge. We aimed to identify somatic mutations associated with lateral neck lymph node (LN) metastasis (N1b) in patients with PTMC.
Methods
Whole-exome sequencing (WES) of 14 PTMCs with no LN metastasis (N0) and 13 N1b PTMCs was performed using primary tumors and matched normal thyroid tissues.
Results
The mutational burden was comparable in N0 and N1b tumors, as the median number of mutations was 23 (range, 12 to 46) in N0 and 24 (range, 12 to 50) in N1b PTMC (P=0.918). The most frequent mutations were detected in PGS1, SLC4A8, DAAM2, and HELZ in N1b PTMCs alone, and the K158Q mutation in PGS1 (four patients, Fisher’s exact test P=0.041) was significantly enriched in N1b PTMCs. Based on pathway analysis, somatic mutations belonging to the receptor tyrosine kinase-RAS and NOTCH pathways were most frequently affected in N1b PTMCs. We identified four mutations that are predicted to be pathogenic in four genes based on Clinvar and Combined Annotation-Dependent Depletion score: BRAF, USH2A, CFTR, and PHIP. A missense mutation in CFTR and a nonsense mutation in PHIP were detected in N1b PTMCs only, although in one case each. BRAF mutation was detected in both N0 and N1b PTMCs.
Conclusion
This first comprehensive WES analysis of the mutational landscape of N0 and N1b PTMCs identified pathogenic genes that affect biological functions associated with the aggressive phenotype of PTMC. -
Citations
Citations to this article as recorded by- What can we learn about acid-base transporters in cancer from studying somatic mutations in their genes?
Bobby White, Pawel Swietach
Pflügers Archiv - European Journal of Physiology.2024; 476(4): 673. CrossRef - Comprehensive Long-Read Sequencing Analysis Discloses the Transcriptome Features of Papillary Thyroid Microcarcinoma
Yanqiang Wang, Binbin Zou, Yanyan Zhang, Jin Zhang, Shujing Li, Bo Yu, Zhekun An, Lei Li, Siqian Cui, Yutong Zhang, Jiali Yao, Xiuzhi Shi, Jing Liu
The Journal of Clinical Endocrinology & Metabolism.2024; 109(5): 1263. CrossRef - Feasibility of whole‐exome sequencing in fine‐needle aspiration specimens of papillary thyroid microcarcinoma for the identification of novel gene mutations
Liyuan Ma, Luying Gao, Ya Hu, Xiaoyi Li, Chunhao Liu, Jiang Ji, Xinlong Shi, Aonan Pan, Yuang An, Nengwen Luo, Yu Xia, Yuxin Jiang
Clinical Genetics.2024; 105(5): 567. CrossRef - Multi-omics analysis reveals a molecular landscape of the early recurrence and early metastasis in pan-cancer
Dan-ni He, Na Wang, Xiao-Ling Wen, Xu-Hua Li, Yu Guo, Shu-heng Fu, Fei-fan Xiong, Zhe-yu Wu, Xu Zhu, Xiao-ling Gao, Zhen-zhen Wang, Hong-jiu Wang
Frontiers in Genetics.2023;[Epub] CrossRef
- What can we learn about acid-base transporters in cancer from studying somatic mutations in their genes?

- Thyroid
- The Concept of Economic Evaluation and Its Application in Thyroid Cancer Research
- Kyungsik Kim, Mijin Kim, Woojin Lim, Bo Hyun Kim, Sue K. Park
- Endocrinol Metab. 2021;36(4):725-736. Published online August 27, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1164
- 4,370 View
- 147 Download
- 3 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
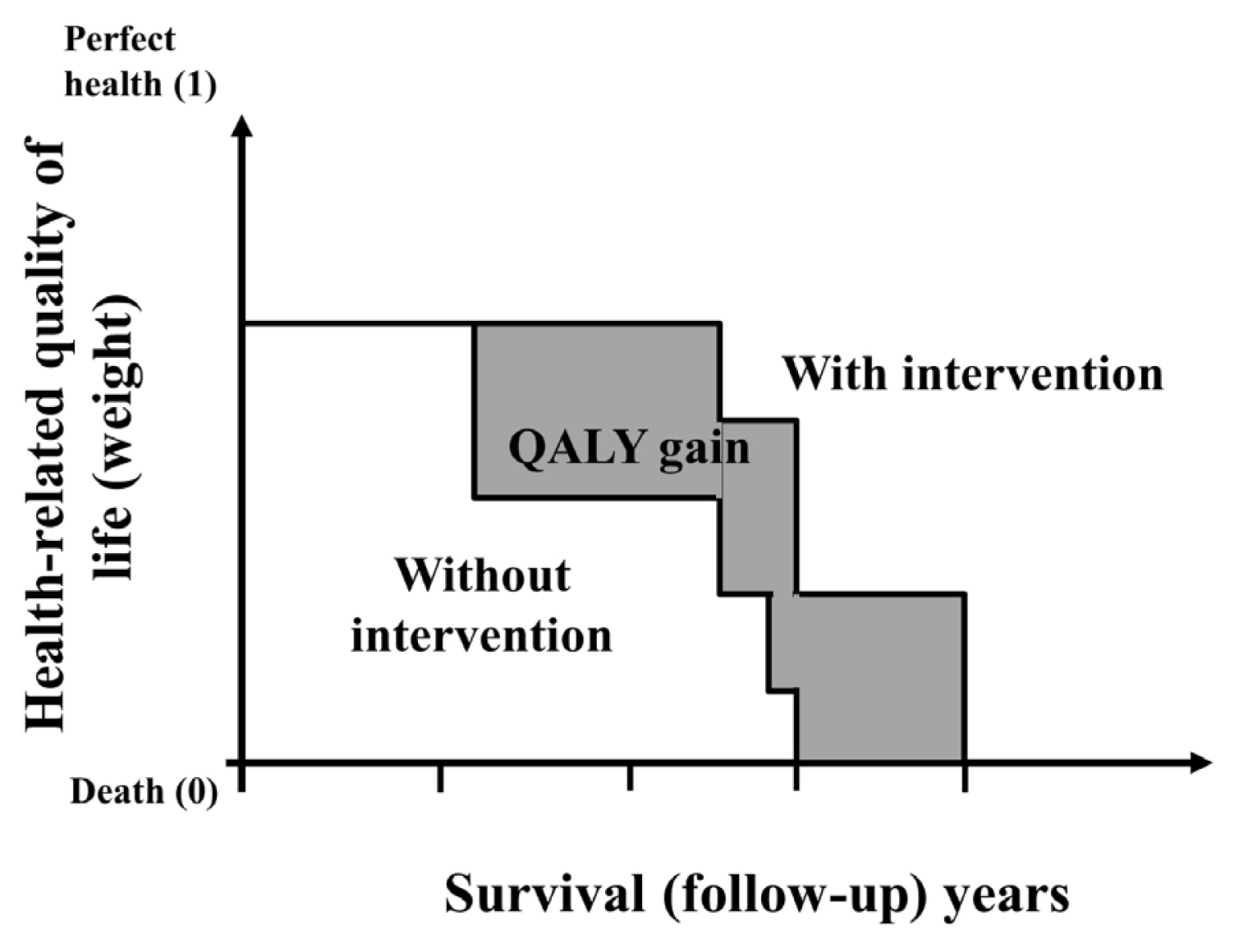
ePub - Economic evaluation is a type of comparative analysis between interventions in terms of both their resource use and health outcomes. Due to the good prognosis of thyroid cancer (TC), the socioeconomic burden of TC patients post-diagnosis is increasing. Therefore, economic evaluation studies focusing on TC are recommended. This study aimed to describe the concept and methods of economic evaluation and reviewed previous TC studies. Several previous studies compared the costs of interventions or evaluated recurrence, complications, or quality of life as measures of their effectiveness. Regarding costs, most studies focused on direct costs and applied hypothetical models. Cost-minimization analysis should be distinguished from simple cost analysis. Furthermore, due to the universality of the term “cost-effectiveness analysis” (CEA), several studies have not distinguished CEA from cost-utility analysis; this point needs to be considered in future research. Cost-benefit analyses have not been conducted in previous TC research. Since TC has a high survival rate and good prognosis, the need for economic evaluations has recently been pointed out. Therefore, correct concepts and methods are needed to obtain clear economic evaluation results. On this basis, it will be possible to provide appropriate guidelines for TC treatment and management in the future.
-
Citations
Citations to this article as recorded by- Cost-Utility Analysis of Early Detection with Ultrasonography of Differentiated Thyroid Cancer: A Retrospective Study on a Korean Population
Han-Sang Baek, Jeonghoon Ha, Kwangsoon Kim, Ja Seong Bae, Jeong Soo Kim, Sungju Kim, Dong-Jun Lim, Chul-Min Kim
Endocrinology and Metabolism.2024; 39(2): 310. CrossRef - Role of Prehabilitation and Rehabilitation on Functional Recovery and Quality of Life in Thyroid Cancer Patients: A Comprehensive Review
Lorenzo Lippi, Alessio Turco, Stefano Moalli, Marco Gallo, Claudio Curci, Antonio Maconi, Alessandro de Sire, Marco Invernizzi
Cancers.2023; 15(18): 4502. CrossRef - Sex-specific Associations between Body Mass Index and Thyroid Cancer Incidence among Korean Adults
Kyoung-Nam Kim, Kyungsik Kim, Sangjun Lee, Sue K. Park
Cancer Epidemiology, Biomarkers & Prevention.2023; 32(9): 1227. CrossRef - Active Surveillance Versus Immediate Surgery for Low-Risk Papillary Thyroid Microcarcinoma Patients in South Korea: A Cost-Minimization Analysis from the MAeSTro Study
Kyungsik Kim, June Young Choi, Su-jin Kim, Eun Kyung Lee, Young Ki Lee, Jun Sun Ryu, Kyu Eun Lee, Jae Hoon Moon, Young Joo Park, Sun Wook Cho, Sue K. Park
Thyroid.2022; 32(6): 648. CrossRef - A Systematic Review of Economic Evaluation of Thyroid Cancer
Mijin Kim, Woojin Lim, Kyungsik Kim, Ja Seong Bae, Byung Joo Lee, Bon Seok Koo, Eun Kyung Lee, Eu Jeong Ku, June Young Choi, Bo Hyun Kim, Sue K. Park
International Journal of Thyroidology.2022; 15(2): 74. CrossRef
- Cost-Utility Analysis of Early Detection with Ultrasonography of Differentiated Thyroid Cancer: A Retrospective Study on a Korean Population

- Thyroid
- Current Guidelines for Management of Medullary Thyroid Carcinoma
- Mijin Kim, Bo Hyun Kim
- Endocrinol Metab. 2021;36(3):514-524. Published online June 22, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1082
- 17,991 View
- 1,711 Download
- 29 Web of Science
- 33 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
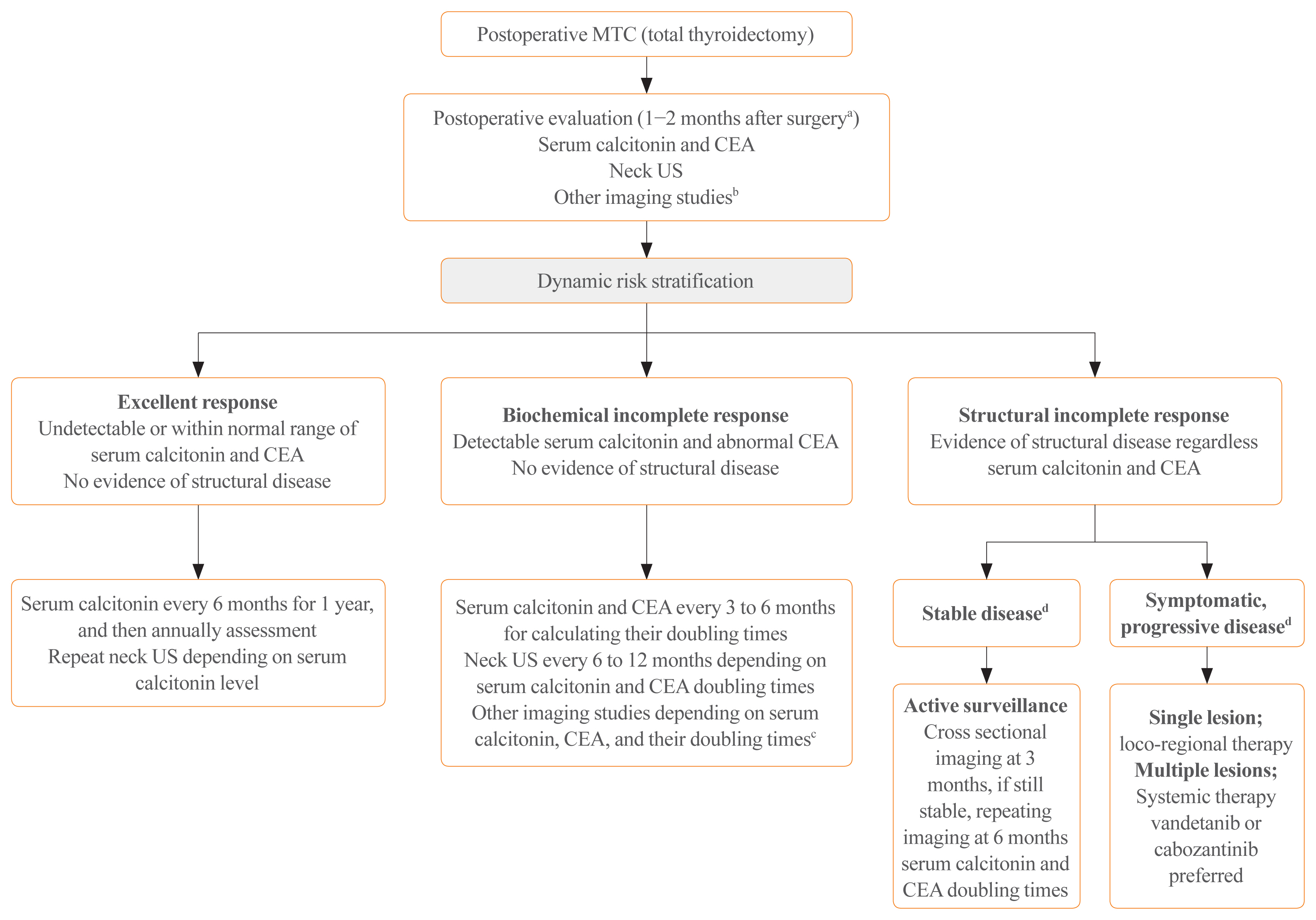
ePub - Medullary thyroid carcinoma (MTC) is a rare neuroendocrine tumor originating from the parafollicular cells. The diagnostic and therapeutic strategies for the condition are different from those used for well-differentiated thyroid cancer. Since the 2015 American Thyroid Association guidelines for the diagnosis and treatment of MTC, the latest, including the National Comprehensive Cancer Network and European Association for Medical Oncology guidelines have been updated to reflect several recent advances in the management of MTC. Advances in molecular diagnosis and postoperative risk stratification systems have led to individualized treatment and follow-up strategies. Multi-kinase inhibitors, such as vandetanib and cabozantinib, can prolong disease progression-free survival with favorable adverse effects. In addition, potent selective rearranged during transfection (RET) inhibitors (selpercatinib and pralsetinib) have shown a promising efficacy in recent clinical trials. This review summarizes the management of MTC in recent guidelines focused on sporadic MTC.
-
Citations
Citations to this article as recorded by- Molecular imaging and related therapeutic options for medullary thyroid carcinoma: state of the art and future opportunities
Alessio Imperiale, Valentina Berti, Mickaël Burgy, Roberto Luigi Cazzato, Arnoldo Piccardo, Giorgio Treglia
Reviews in Endocrine and Metabolic Disorders.2024; 25(1): 187. CrossRef - Diffuse C-Cells Hyperplasia Is the Source of False Positive Calcitonin Measurement in FNA Washout Fluids of Thyroid Nodules: A Rational Clinical Approach to Avoiding Unnecessary Surgery
Chiara Mura, Rossella Rodia, Silvia Corrias, Antonello Cappai, Maria Letizia Lai, Gian Luigi Canu, Fabio Medas, Pietro Giorgio Calò, Stefano Mariotti, Francesco Boi
Cancers.2024; 16(1): 210. CrossRef - Meta-Analysis of the Efficacy and Safety Evaluation of Vandetanib in
the Treatment of Medullary Thyroid Cancer
Tong-cheng Xian, Min-ye Yang, Xue-lin Zhang, Jie Wang, Yi Luo
Hormone and Metabolic Research.2024;[Epub] CrossRef - Successful localisation of recurrent thyroid cancer using preoperative patent blue dye injection
B. O. Evranos, N. Ince, H. Ataş, S. B. Polat, H. Ahsen, N. N. Imga, A. Dirikoc, O. Topaloglu, T. Tutuncu, R. Ersoy, B. Cakir
Journal of Endocrinological Investigation.2024;[Epub] CrossRef - Current and future of immunotherapy for thyroid cancer based on bibliometrics and clinical trials
Ke Wang, Ying Zhang, Yang Xing, Hong Wang, Minghua He, Rui Guo
Discover Oncology.2024;[Epub] CrossRef - Combining radiomics with thyroid imaging reporting and data system to predict lateral cervical lymph node metastases in medullary thyroid cancer
Zhiqiang Liu, Xiwei Zhang, Xiaohui Zhao, Qianqian Guo, Zhengjiang Li, Minghui Wei, Lijuan Niu, Changming An
BMC Medical Imaging.2024;[Epub] CrossRef - Potentials and future perspectives of multi-target drugs in cancer treatment: the next generation anti-cancer agents
Ali Doostmohammadi, Hossein Jooya, Kimia Ghorbanian, Sargol Gohari, Mehdi Dadashpour
Cell Communication and Signaling.2024;[Epub] CrossRef - Diagnostic capabilities of PET/CT with 18F-DOPA in biochemical recurrence of medullary thyroid carcinoma: a retrospective study
N. V. Tsentr, A. A. Zyryanova, M. A. Rusnak, D. V. Ryzhkova
Diagnostic radiology and radiotherapy.2024; 15(1): 87. CrossRef - LINC00887 Acts as an Enhancer RNA to Promote Medullary Thyroid
Carcinoma Progression by Binding with FOXQ1
Daxiang Liu, Wenjing Wang, Yanzhao Wu, Yongle Qiu, Lan Zhang
Current Cancer Drug Targets.2024; 24(5): 519. CrossRef - Update on Management of Medullary Thyroid Carcinoma: Focus on Nuclear Medicine
Giorgio Treglia, Vittoria Rufini, Arnoldo Piccardo, Alessio Imperiale
Seminars in Nuclear Medicine.2023; 53(4): 481. CrossRef - Cabozantinib, Vandetanib, Pralsetinib and Selpercatinib as Treatment for Progressed Medullary Thyroid Cancer with a Main Focus on Hypertension as Adverse Effect
Linnea Højer Wang, Markus Wehland, Petra M. Wise, Manfred Infanger, Daniela Grimm, Michael C. Kreissl
International Journal of Molecular Sciences.2023; 24(3): 2312. CrossRef - A proposed grading scheme for predicting recurrence in medullary thyroid cancer based on the Ki67 index and metastatic lymph node ratio
Pengfei Xu, Di Wu, Xuekui Liu
Endocrine.2023; 81(1): 107. CrossRef - Efficacy and Safety of [177Lu]Lu-DOTA-TATE in Adults with Inoperable or Metastatic Somatostatin Receptor-Positive Pheochromocytomas/Paragangliomas, Bronchial and Unknown Origin Neuroendocrine Tumors, and Medullary Thyroid Carcinoma: A Systematic Literatur
Marianna Hertelendi, Oulaya Belguenani, Azzeddine Cherfi, Ilya Folitar, Gabor Kollar, Berna Degirmenci Polack
Biomedicines.2023; 11(4): 1024. CrossRef - PET/CT with various radiopharmaceuticals in the complex diagnosis of medullary thyroid carcinoma: a review
N. V. Tsentr, A. E. Ertman, D. V. Ryzhkova
Diagnostic radiology and radiotherapy.2023; 14(2): 31. CrossRef - Physical activity and reduced risk of fracture in thyroid cancer patients after thyroidectomy — a nationwide cohort study
Jinyoung Kim, Kyungdo Han, Jin-Hyung Jung, Jeonghoon Ha, Chaiho Jeong, Jun-Young Heu, Se-Won Lee, Jeongmin Lee, Yejee Lim, Mee Kyoung Kim, Hyuk-Sang Kwon, Ki-Ho Song, Ki-Hyun Baek
Frontiers in Endocrinology.2023;[Epub] CrossRef - Different RONS Generation in MTC-SK and NSCL Cells Lead to Varying Antitumoral Effects of Alpha-Ketoglutarate + 5-HMF
Joachim Greilberger, Katharina Erlbacher, Philipp Stiegler, Reinhold Wintersteiger, Ralf Herwig
Current Issues in Molecular Biology.2023; 45(8): 6503. CrossRef - Medullary thyroid carcinoma
Maria Rosa Pelizzo, Esmeralda Isabella Mazza, Caterina Mian, Isabella Merante Boschin
Expert Review of Anticancer Therapy.2023; 23(9): 943. CrossRef - Mixed medullary‑follicular thyroid carcinoma: A case report and literature review
Yonghui Wang, Dandan Yin, Guifang Ren, Zhengjiang Wang, Fanhua Kong
Oncology Letters.2023;[Epub] CrossRef - Circulating cell-free DNA (cfDNA) in patients with medullary thyroid carcinoma is characterized by specific fragmentation and methylation changes with diagnostic value
Anna Citarella, Zein Mersini Besharat, Sofia Trocchianesi, Tanja Milena Autilio, Antonella Verrienti, Giuseppina Catanzaro, Elena Splendiani, Zaira Spinello, Silvia Cantara, Patrizia Zavattari, Eleonora Loi, Cristina Romei, Raffaele Ciampi, Luciano Pezzul
Biomarker Research.2023;[Epub] CrossRef - Advances in Diagnostics and Therapy of Medullary Thyroid Carcinoma (MTC)– A Mini-Review
Michał Miciak, Krzysztof Jurkiewicz
Clinical Cancer Investigation Journal.2023; 12(5): 1. CrossRef - The Evolving Treatment Landscape of Medullary Thyroid Cancer
Marta Laganà, Valentina Cremaschi, Andrea Alberti, Danica M. Vodopivec Kuri, Deborah Cosentini, Alfredo Berruti
Current Treatment Options in Oncology.2023; 24(12): 1815. CrossRef - Pralsetinib: chemical and therapeutic development with FDA authorization for the management of RET fusion-positive non-small-cell lung cancers
Faraat Ali, Kumari Neha, Garima Chauhan
Archives of Pharmacal Research.2022; 45(5): 309. CrossRef - Psychosocial Characteristics and Experiences in Patients with Multiple Endocrine Neoplasia Type 2 (MEN2) and Medullary Thyroid Carcinoma (MTC)
Robin Lockridge, Sima Bedoya, Taryn Allen, Brigitte Widemann, Srivandana Akshintala, John Glod, Lori Wiener
Children.2022; 9(6): 774. CrossRef - Aggressive clinical course of medullary thyroid microcarcinoma
Tamara Janić, Mirjana Stojković, Sanja Klet, Bojan Marković, Beleslin Nedeljković, Jasmina Ćirić, Miloš Žarković
Medicinski glasnik Specijalne bolnice za bolesti štitaste žlezde i bolesti metabolizma.2022; 27(85): 63. CrossRef - Comparative evaluation of somatostatin and CXCR4 receptor expression in different types of thyroid carcinoma using well-characterised monoclonal antibodies
Max Czajkowski, Daniel Kaemmerer, Jörg Sänger, Guido Sauter, Ralph M. Wirtz, Stefan Schulz, Amelie Lupp
BMC Cancer.2022;[Epub] CrossRef - Metastatic Risk Stratification of 2526 Medullary Thyroid Carcinoma Patients: A Study Based on Surveillance, Epidemiology, and End Results Database
Minh-Khang Le, Masataka Kawai, Toru Odate, Huy Gia Vuong, Naoki Oishi, Tetsuo Kondo
Endocrine Pathology.2022; 33(3): 348. CrossRef - Update on the Diagnosis and Management of Medullary Thyroid Cancer: What Has Changed in Recent Years?
Krzysztof Kaliszewski, Maksymilian Ludwig, Bartłomiej Ludwig, Agnieszka Mikuła, Maria Greniuk, Jerzy Rudnicki
Cancers.2022; 14(15): 3643. CrossRef - Immunotherapy of Neuroendocrine Neoplasms: Any Role for the Chimeric Antigen Receptor T Cells?
Giuseppe Fanciulli, Roberta Modica, Anna La Salvia, Federica Campolo, Tullio Florio, Nevena Mikovic, Alice Plebani, Valentina Di Vito, Annamaria Colao, Antongiulio Faggiano
Cancers.2022; 14(16): 3991. CrossRef - Preclinical Evaluation of Novel Tyrosine-Kinase Inhibitors in Medullary Thyroid Cancer
Davide Saronni, Germano Gaudenzi, Alessandra Dicitore, Silvia Carra, Maria Celeste Cantone, Maria Orietta Borghi, Andrea Barbieri, Luca Mignani, Leo J. Hofland, Luca Persani, Giovanni Vitale
Cancers.2022; 14(18): 4442. CrossRef - Rapid and long-lasting response to selpercatinib of paraneoplastic Cushing’s syndrome in medullary thyroid carcinoma
Marine Sitbon, Porhuoy Chou, Seydou Bengaly, Brigitte Poirot, Marie Laloi-Michelin, Laure Deville, Atanas Pachev, Ahouefa Kowo-Bille, Clement Dumont, Cécile N Chougnet
European Thyroid Journal.2022;[Epub] CrossRef - Ginsenoside Rg3 Alleviates Antithyroid Cancer Drug Vandetanib-Induced QT Interval Prolongation
Juan Zhang, Dan Luo, Fang Li, Zhiyi Li, Xiaoli Gao, Jie Qiao, Lin Wu, Miaoling Li, Shao Liang
Oxidative Medicine and Cellular Longevity.2021; 2021: 1. CrossRef - THE ROLE OF CALCITONIN IN THE PREOPERATIVE STAGE AS THE PREDICTOR OF MEDULLARY THYROID CANCER METASTASES
Volodymyr Palamarchuk , Viktor Smolyar , Oleksandr Tovkay, Oleksandr Nechay, Volodymyr Kuts , Revaz Sichinava , Oleh Mazur
Ukrainian Scientific Medical Youth Journal.2021; 127(4): 68. CrossRef - THE ROLE OF CALCITONIN IN THE PREOPERATIVE STAGE AS THE PREDICTOR OF MEDULLARY THYROID CANCER METASTASES
Volodymyr Palamarchuk , Viktor Smolyar , Oleksandr Tovkay , Oleksandr Nechay , Volodymyr Kuts , Revaz Sichinava , Oleh Mazur
The Ukrainian Scientific Medical Youth Journal.2021; 4(127): 68. CrossRef
- Molecular imaging and related therapeutic options for medullary thyroid carcinoma: state of the art and future opportunities

- Thyroid
- Clinicopathological Characteristics and Recurrence-Free Survival of Rare Variants of Papillary Thyroid Carcinomas in Korea: A Retrospective Study
- Mijin Kim, Sun Wook Cho, Young Joo Park, Hwa Young Ahn, Hee Sung Kim, Yong Joon Suh, Dughyun Choi, Bu Kyung Kim, Go Eun Yang, Il-Seok Park, Ka Hee Yi, Chan Kwon Jung, Bo Hyun Kim
- Endocrinol Metab. 2021;36(3):619-627. Published online June 10, 2021
- DOI: https://doi.org/10.3803/EnM.2021.974
- 4,698 View
- 180 Download
- 6 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
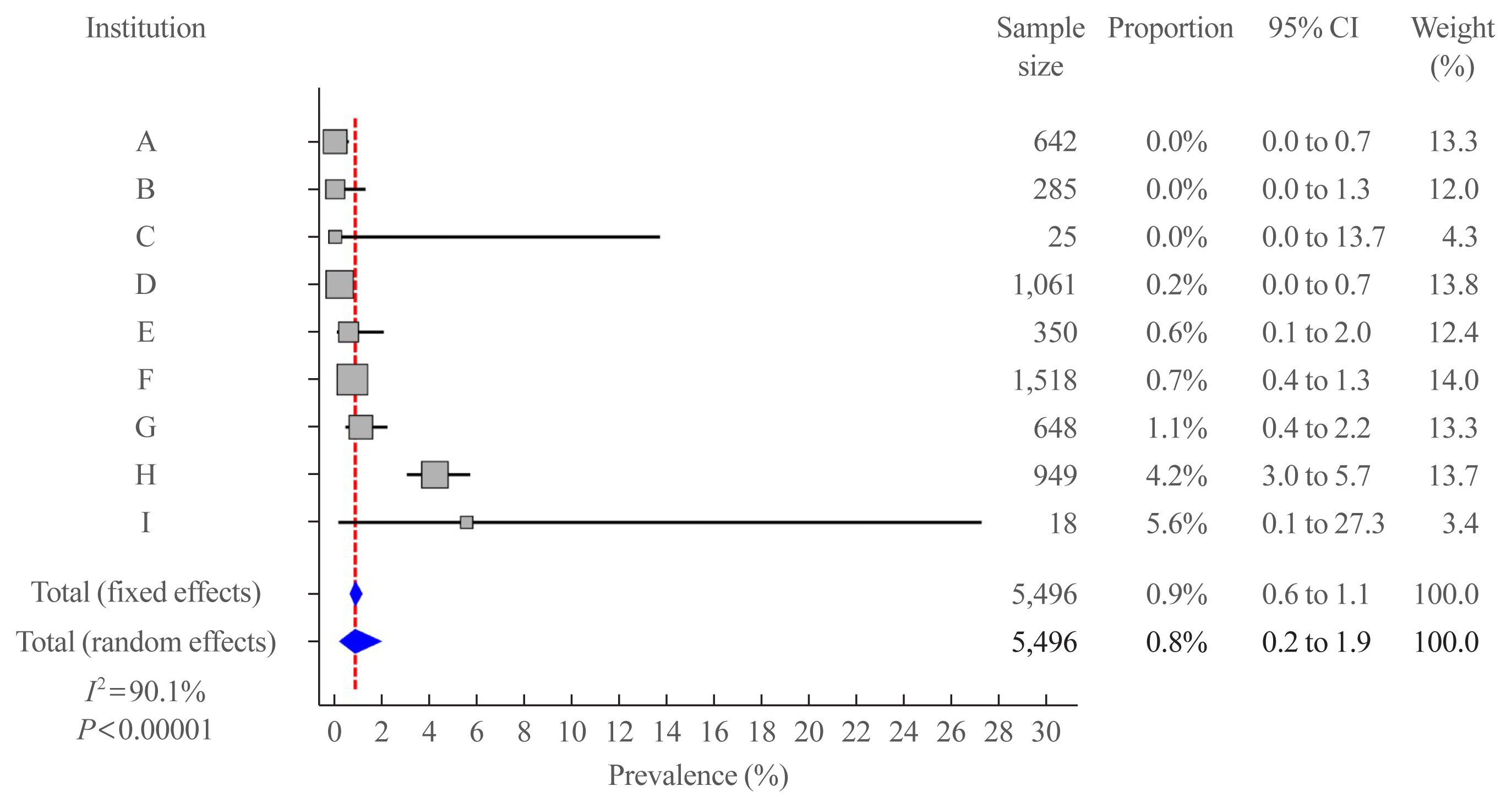
We aimed to evaluate the clinicopathological features and biological behaviors of Korean thyroid cancer patients with rare variants of papillary thyroid carcinoma (PTC) to address the ambiguity regarding the prognostic consequences of these variants.
Methods
We retrospectively reviewed the medical records of 5,496 patients who underwent thyroid surgery for PTC, between January and December 2012, in nine tertiary hospitals. Rare PTC variants included tall cell (TCV), columnar cell (CCV), diffuse sclerosing (DSV), cribriform-morular (CMV), solid (SV), hobnail, and Warthin-like variants. Recurrence-free survival (RFS) was defined as the time from the date of thyroidectomy until recurrence.
Results
Rare variants accounted for 1.1% (n=63) of the PTC patients; with 0.9% TCV, 0.02% CCV, 0.1% DSV, 0.1% CMV, and 0.1% SV. The mean age of patients and primary tumor size were 42.1±13.1 years and 1.3±0.9 cm, respectively. Extrathyroidal extension and cervical lymph node metastasis were observed in 38 (60.3%) and 37 (58.7%) patients, respectively. Ultrasonographic findings revealed typical malignant features in most cases. During a median follow-up of 7 years, 6.3% of patients experienced a locoregional recurrence. The 5-year RFS rates were 71.4% in patients with DSV or SV, 95.9% for TCV, or CCV, and 100% for other variants. DSV emerged an independent risk factor associated with shorter RFS.
Conclusion
In this multicenter Korean cohort, rare variants accounted for 1.1% of all PTC cases, with TCV being the most frequent subtype. DSV emerged as a significant prognostic factor for RFS. -
Citations
Citations to this article as recorded by- Serum thyroglobulin testing after thyroid lobectomy in patients with 1–4 cm papillary thyroid carcinoma
Ahreum Jang, Meihua Jin, Chae A Kim, Min Ji Jeon, Yu-Mi Lee, Tae-Yon Sung, Tae Yong Kim, Won Bae Kim, Young Kee Shong, Won Gu Kim
Endocrine.2023; 81(2): 290. CrossRef - Do Histologically Aggressive Subtypes of Papillary Thyroid
Microcarcinoma have Worse Clinical Outcome than Non-Aggressive Papillary Thyroid
Microcarcinoma Subtypes? A Multicenter Cohort Study
Sayid Shafi Zuhur, Hunkar Aggul, Ugur Avci, Selvinaz Erol, Mazhar Müslüm Tuna, Serhat Uysal, Gulhan Akbaba, Faruk Kilinç, Merve Catak, Sakin Tekin, Ogun Irem Bilen, Beyza Olcay Öztürk, Ecem Bilgehan Erden, Gulsah Elbuken, Halise Cinar Yavuz, Pinar Kadiogl
Hormone and Metabolic Research.2023; 55(05): 323. CrossRef - The Warthin-like variant of papillary thyroid carcinomas: a clinicopathologic analysis report of two cases
Xing Zhao, Yijia Zhang, Pengyu Hao, Mingzhen Zhao, Xingbin Shen
Oncologie.2023; 25(5): 581. CrossRef - A Retrospective Cohort Study with Validation of Predictors of Differentiated Thyroid Cancer Outcomes
Ayanthi Wijewardene, Anthony J. Gill, Matti Gild, Diana L. Learoyd, Anthony Robert Glover, Mark Sywak, Stan Sidhu, Paul Roach, Geoffrey Schembri, Jeremy Hoang, Bruce Robinson, Lyndal Tacon, Roderick Clifton-Bligh
Thyroid.2022;[Epub] CrossRef - Clinicopathological Implications of the BRAFV600E Mutation in Papillary Thyroid Carcinoma of Ukrainian Patients Exposed to the Chernobyl Radiation in Childhood: A Study for 30 Years After the Accident
Liudmyla Zurnadzhy, Tetiana Bogdanova, Tatiana I. Rogounovitch, Masahiro Ito, Mykola Tronko, Shunichi Yamashita, Norisato Mitsutake, Michael Bolgov, Serhii Chernyshov, Sergii Masiuk, Vladimir A. Saenko
Frontiers in Medicine.2022;[Epub] CrossRef
- Serum thyroglobulin testing after thyroid lobectomy in patients with 1–4 cm papillary thyroid carcinoma

- Thyroid
- A Multicenter, Randomized, Controlled Trial for Assessing the Usefulness of Suppressing Thyroid Stimulating Hormone Target Levels after Thyroid Lobectomy in Low to Intermediate Risk Thyroid Cancer Patients (MASTER): A Study Protocol
- Eun Kyung Lee, Yea Eun Kang, Young Joo Park, Bon Seok Koo, Ki-Wook Chung, Eu Jeong Ku, Ho-Ryun Won, Won Sang Yoo, Eonju Jeon, Se Hyun Paek, Yong Sang Lee, Dong Mee Lim, Yong Joon Suh, Ha Kyoung Park, Hyo-Jeong Kim, Bo Hyun Kim, Mijin Kim, Sun Wook Kim, Ka Hee Yi, Sue K. Park, Eun-Jae Jung, June Young Choi, Ja Seong Bae, Joon Hwa Hong, Kee-Hyun Nam, Young Ki Lee, Hyeong Won Yu, Sujeong Go, Young Mi Kang, MASTER study group
- Endocrinol Metab. 2021;36(3):574-581. Published online May 26, 2021
- DOI: https://doi.org/10.3803/EnM.2020.943
- 6,294 View
- 268 Download
- 8 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
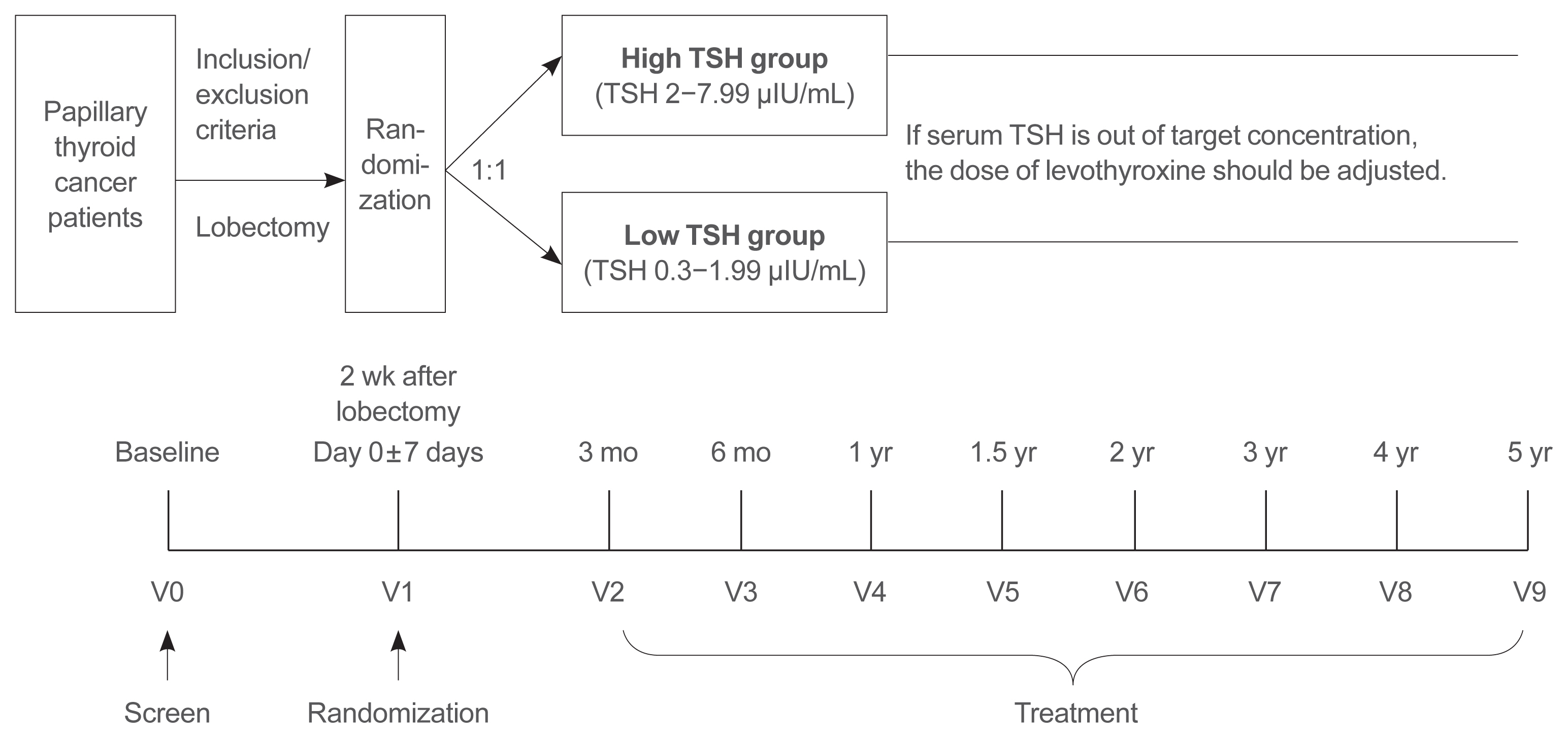
Postoperative thyroid stimulating hormone (TSH) suppression therapy is recommended for patients with intermediate- and high-risk differentiated thyroid cancer to prevent the recurrence of thyroid cancer. With the recent increase in small thyroid cancer cases, the extent of resection during surgery has generally decreased. Therefore, questions have been raised about the efficacy and long-term side effects of TSH suppression therapy in patients who have undergone a lobectomy.
Methods
This is a multicenter, prospective, randomized, controlled clinical trial in which 2,986 patients with papillary thyroid cancer are randomized into a high-TSH group (intervention) and a low-TSH group (control) after having undergone a lobectomy. The principle of treatment includes a TSH-lowering regimen aimed at TSH levels between 0.3 and 1.99 μIU/mL in the low-TSH group. The high-TSH group targets TSH levels between 2.0 and 7.99 μIU/mL. The dose of levothyroxine will be adjusted at each visit to maintain the target TSH level. The primary outcome is recurrence-free survival, as assessed by neck ultrasound every 6 to 12 months. Secondary endpoints include disease-free survival, overall survival, success rate in reaching the TSH target range, the proportion of patients with major cardiovascular diseases or bone metabolic disease, the quality of life, and medical costs. The follow-up period is 5 years.
Conclusion
The results of this trial will contribute to establishing the optimal indication for TSH suppression therapy in low-risk papillary thyroid cancer patients by evaluating the benefit and harm of lowering TSH levels in terms of recurrence, metabolic complications, costs, and quality of life. -
Citations
Citations to this article as recorded by- Effect of thyroid-stimulating hormone suppression on quality of life in thyroid lobectomy patients: interim analysis of a multicenter, randomized controlled trial in low- to intermediate-risk thyroid cancer patients (MASTER study)
Ja Kyung Lee, Eu Jeong Ku, Su-jin Kim, Woochul Kim, Jae Won Cho, Kyong Yeun Jung, Hyeong Won Yu, Yea Eun Kang, Mijin Kim, Hee Kyung Kim, Junsun Ryu, June Young Choi
Annals of Surgical Treatment and Research.2024; 106(1): 19. CrossRef - Clinical impact of coexistent chronic lymphocytic thyroiditis on central lymph node metastasis in low- to intermediate-risk papillary thyroid carcinoma: The MASTER study
Da Beom Heo, Ho-Ryun Won, Kyung Tae, Yea Eun Kang, Eonju Jeon, Yong Bae Ji, Jae Won Chang, June Young Choi, Hyeong Won Yu, Eu Jeong Ku, Eun Kyung Lee, Mijin Kim, Jun-Ho Choe, Bon Seok Koo
Surgery.2024; 175(4): 1049. CrossRef - Dynamic Changes in Treatment Response af-ter 131I in Differentiated Thyroid Cancer and Their Relationship with Recurrence Risk Stratification and TNM Staging
璐 狄
Advances in Clinical Medicine.2024; 14(03): 1083. CrossRef - ASO Author Reflections: Active Surveillance may be Possible in Patients with T1b Papillary Thyroid Carcinoma Over 55 Years of Age Without High-Risk Features on Preoperative Examinations
Ho-Ryun Won, Eonju Jeon, Da Beom Heo, Jae Won Chang, Minho Shong, Je Ryong Kim, Hyemi Ko, Yea Eun Kang, Hyon-Seung Yi, Ju Hee Lee, Kyong Hye Joung, Ji Min Kim, Younju Lee, Sung-Woo Kim, Young Ju Jeong, Yong Bae Ji, Kyung Tae, Bon Seok Koo
Annals of Surgical Oncology.2023; 30(4): 2254. CrossRef - Outcomes and Trends of Treatments in High‐Risk Differentiated Thyroid Cancer
Arash Abiri, Khodayar Goshtasbi, Sina J. Torabi, Edward C. Kuan, William B. Armstrong, Tjoson Tjoa, Yarah M. Haidar
Otolaryngology–Head and Neck Surgery.2023; 168(4): 745. CrossRef - Current Controversies in Low-Risk Differentiated Thyroid Cancer: Reducing Overtreatment in an Era of Overdiagnosis
Timothy M Ullmann, Maria Papaleontiou, Julie Ann Sosa
The Journal of Clinical Endocrinology & Metabolism.2023; 108(2): 271. CrossRef - Age-Dependent Clinicopathological Characteristics of Patients with T1b Papillary Thyroid Carcinoma: Implications for the Possibility of Active Surveillance
Ho-Ryun Won, Eonju Jeon, Da Beom Heo, Jae Won Chang, Minho Shong, Je Ryong Kim, Hyemi Ko, Yea Eun Kang, Hyon-Seung Yi, Ju Hee Lee, Kyong Hye Joung, Ji Min Kim, Younju Lee, Sung-Woo Kim, Young Ju Jeong, Yong Bae Ji, Kyung Tae, Bon Seok Koo
Annals of Surgical Oncology.2023; 30(4): 2246. CrossRef - Potential impact of obesity on the aggressiveness of low- to intermediate-risk papillary thyroid carcinoma: results from a MASTER cohort study
Mijin Kim, Yae Eun Kang, Young Joo Park, Bon Seok Koo, Eu Jeong Ku, June Young Choi, Eun Kyung Lee, Bo Hyun Kim
Endocrine.2023; 82(1): 134. CrossRef - Differentiated thyroid cancer: a focus on post-operative thyroid hormone replacement and thyrotropin suppression therapy
Benjamin J. Gigliotti, Sina Jasim
Endocrine.2023; 83(2): 251. CrossRef - Thyroid stimulating hormone suppression and recurrence after thyroid lobectomy for papillary thyroid carcinoma
Mi Rye Bae, Sung Hoon Nam, Jong-Lyel Roh, Seung-Ho Choi, Soon Yuhl Nam, Sang Yoon Kim
Endocrine.2022; 75(2): 487. CrossRef - The Concept of Economic Evaluation and Its Application in Thyroid Cancer Research
Kyungsik Kim, Mijin Kim, Woojin Lim, Bo Hyun Kim, Sue K. Park
Endocrinology and Metabolism.2021; 36(4): 725. CrossRef
- Effect of thyroid-stimulating hormone suppression on quality of life in thyroid lobectomy patients: interim analysis of a multicenter, randomized controlled trial in low- to intermediate-risk thyroid cancer patients (MASTER study)

- Clinical Study
- Protocol for a Korean Multicenter Prospective Cohort Study of Active Surveillance or Surgery (KoMPASS) in Papillary Thyroid Microcarcinoma
- Min Ji Jeon, Yea Eun Kang, Jae Hoon Moon, Dong Jun Lim, Chang Yoon Lee, Yong Sang Lee, Sun Wook Kim, Min-Hee Kim, Bo Hyun Kim, Ho-Cheol Kang, Minho Shong, Sun Wook Cho, Won Bae Kim
- Endocrinol Metab. 2021;36(2):359-364. Published online March 23, 2021
- DOI: https://doi.org/10.3803/EnM.2020.890
- Correction in: Endocrinol Metab 2022;37(1):181
- 5,799 View
- 202 Download
- 17 Web of Science
- 17 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
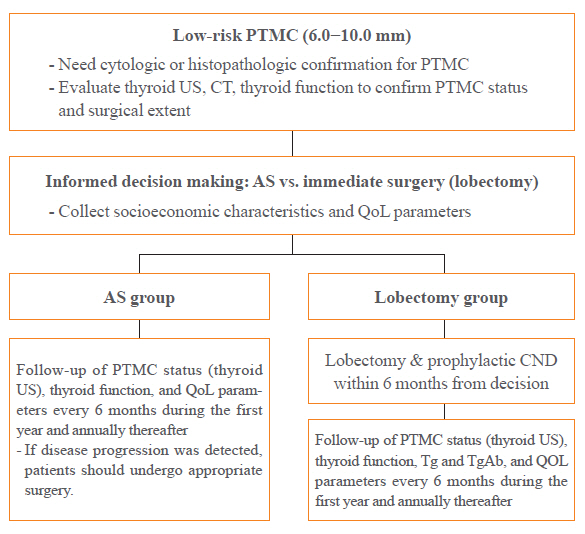
A Korean Multicenter Prospective cohort study of Active Surveillance or Surgery (KoMPASS) for papillary thyroid microcarcinomas (PTMCs) has been initiated. The aim is to compare clinical outcomes between active surveillance (AS) and an immediate lobectomy for low-risk PTMCs. We here outline the detailed protocol for this study.
Methods
Adult patients with a cytopathologically confirmed PTMC sized 6.0 to 10.0 mm by ultrasound (US) will be included. Patients will be excluded if they have a suspicious extra-thyroidal extension or metastasis of a PTMC or multiple thyroid nodules or other thyroid diseases which require a total thyroidectomy. Printed material describing the prognosis of PTMCs, and the pros and cons of each management option, will be provided to eligible patients to select their preferred intervention. For the AS group, thyroid US, thyroid function, and quality of life (QoL) parameters will be monitored every 6 months during the first year, and then annually thereafter. Disease progression will be defined as a ≥3 mm increase in maximal diameter of a PTMC, or the development of new thyroid cancers or metastases. If progression is detected, patients should undergo appropriate surgery. For the lobectomy group, a lobectomy with prophylactic central neck dissection will be done within 6 months. After initial surgery, thyroid US, thyroid function, serum thyroglobulin (Tg), anti-Tg antibody, and QoL parameters will be monitored every 6 months during the first year and annually thereafter. Disease progression will be defined in these cases as the development of new thyroid cancers or metastases.
Conclusion
KoMPASS findings will help to confirm the role of AS, and develop individualized management strategies, for low-risk PTMCs. -
Citations
Citations to this article as recorded by- Active Surveillance for Low-Risk Thyroid Cancers: A Review of Current Practice Guidelines
Min Joo Kim, Jae Hoon Moon, Eun Kyung Lee, Young Shin Song, Kyong Yeun Jung, Ji Ye Lee, Ji-hoon Kim, Kyungsik Kim, Sue K. Park, Young Joo Park
Endocrinology and Metabolism.2024; 39(1): 47. CrossRef - It Is Time to Understand the Additional Benefits of Active Surveillance for Low-Risk Papillary Thyroid Carcinoma
Kyeong Jin Kim
Endocrinology and Metabolism.2024; 39(1): 95. CrossRef - Active Surveillance for Low-Risk Papillary Thyroid Carcinoma as an Acceptable Management Option with Additional Benefits: A Comprehensive Systematic Review
Jee Hee Yoon, Wonsuk Choi, Ji Yong Park, A Ram Hong, Hee Kyung Kim, Ho-Cheol Kang
Endocrinology and Metabolism.2024; 39(1): 152. CrossRef - Active Surveillance for Low-Risk Papillary Thyroid Carcinoma as an Acceptable Management Option with Additional Benefits: A Comprehensive Systematic Review
Jee Hee Yoon, Wonsuk Choi, Ji Yong Park, A Ram Hong, Hee Kyung Kim, Ho-Cheol Kang
Endocrinology and Metabolism.2024; 39(1): 152. CrossRef - Thyroid‐Stimulating Hormone, Age, and Tumor Size are Risk Factors for Progression During Active Surveillance of Low‐Risk Papillary Thyroid Microcarcinoma in Adults
Yasuhiro Ito, Akira Miyauchi, Makoto Fujishima, Takuya Noda, Tsutomu Sano, Takahiro Sasaki, Taketoshi Kishi, Tomohiko Nakamura
World Journal of Surgery.2023; 47(2): 392. CrossRef - Thyroid FNA cytology: The Eastern versus Western perspectives
Mitsuyoshi Hirokawa, Manon Auger, Chan Kwon Jung, Fabiano Mesquita Callegari
Cancer Cytopathology.2023; 131(7): 415. CrossRef - To Screen or Not to Screen?
Do Joon Park
Endocrinology and Metabolism.2023; 38(1): 69. CrossRef - Lower Thyroid Cancer Mortality in Patients Detected by Screening: A Meta-Analysis
Shinje Moon, Young Shin Song, Kyong Yeun Jung, Eun Kyung Lee, Young Joo Park
Endocrinology and Metabolism.2023; 38(1): 93. CrossRef - Long-Term Outcomes of Active Surveillance and Immediate Surgery for Adult Patients with Low-Risk Papillary Thyroid Microcarcinoma: 30-Year Experience
Akira Miyauchi, Yasuhiro Ito, Makoto Fujishima, Akihiro Miya, Naoyoshi Onoda, Minoru Kihara, Takuya Higashiyama, Hiroo Masuoka, Shiori Kawano, Takahiro Sasaki, Mitsushige Nishikawa, Shuji Fukata, Takashi Akamizu, Mitsuru Ito, Eijun Nishihara, Mako Hisakad
Thyroid®.2023; 33(7): 817. CrossRef - Active Surveillance Outcomes of Patients with Low-Risk Papillary Thyroid Microcarcinoma According to Levothyroxine Treatment Status
Masashi Yamamoto, Akira Miyauchi, Yasuhiro Ito, Makoto Fujishima, Takahiro Sasaki, Takumi Kudo
Thyroid®.2023; 33(10): 1182. CrossRef - Cost-Effectiveness of Active Surveillance Compared to Early Surgery of Small Papillary Thyroid Cancer: A Retrospective Study on a Korean Population
Han-Sang Baek, Jeonghoon Ha, Kwangsoon Kim, Jaseong Bae, Jeong Soo Kim, Sungju Kim, Dong-Jun Lim, Chulmin Kim
Journal of Korean Medical Science.2023;[Epub] CrossRef - Optimal Cutoff Values of the Contact Angle of Tumor on Sonography System for Predicting Extrathyroidal Extension of Papillary Thyroid Carcinoma by Tumor Location
Ik Beom Shin, Do Hoon Koo, Dong Sik Bae
Clinical Medicine Insights: Oncology.2023;[Epub] CrossRef - Thermal ablation for papillary thyroid microcarcinoma located in the isthmus: a study with 3 years of follow-up
Lin Zheng, Fang-yi Liu, Jie Yu, Zhi-gang Cheng, Xiao-ling Yu, Xiao-cong Dong, Zhi-yu Han, Ping Liang
Future Oncology.2022; 18(4): 471. CrossRef - Trends in the Management of Localized Papillary Thyroid Carcinoma in the United States (2000–2018)
Elisa Pasqual, Julie Ann Sosa, Yingxi Chen, Sara J. Schonfeld, Amy Berrington de González, Cari M. Kitahara
Thyroid.2022; 32(4): 397. CrossRef - Management of Low-Risk Thyroid Cancers: Is Active Surveillance a Valid Option? A Systematic Review of the Literature
Renato Patrone, Nunzio Velotti, Stefania Masone, Alessandra Conzo, Luigi Flagiello, Chiara Cacciatore, Marco Filardo, Vincenza Granata, Francesco Izzo, Domenico Testa, Stefano Avenia, Alessandro Sanguinetti, Andrea Polistena, Giovanni Conzo
Journal of Clinical Medicine.2021; 10(16): 3569. CrossRef - Cost-Effectiveness Analysis of Active Surveillance Compared to Early Surgery in Small Papillary Thyroid Cancer: A Systemic Review
Han-sang Baek, Chai-ho Jeong, Jeonghoon Ha, Ja-Seong Bae, Jeong-soo Kim, Dong-Jun Lim, Chul-Min Kim
Cancer Management and Research.2021; Volume 13: 6721. CrossRef - Active Surveillance as an Effective Management Option for Low-Risk Papillary Thyroid Microcarcinoma
Min Ji Jeon, Won Gu Kim, Tae Yong Kim, Young Kee Shong, Won Bae Kim
Endocrinology and Metabolism.2021; 36(4): 717. CrossRef
- Active Surveillance for Low-Risk Thyroid Cancers: A Review of Current Practice Guidelines

- Clinical Study
- Clinical Implication of World Health Organization Classification in Patients with Follicular Thyroid Carcinoma in South Korea: A Multicenter Cohort Study
- Meihua Jin, Eun Sook Kim, Bo Hyun Kim, Hee Kyung Kim, Hyon-Seung Yi, Min Ji Jeon, Tae Yong Kim, Ho-Cheol Kang, Won Bae Kim, Young Kee Shong, Mijin Kim, Won Gu Kim
- Endocrinol Metab. 2020;35(3):618-627. Published online September 22, 2020
- DOI: https://doi.org/10.3803/EnM.2020.742
- 5,402 View
- 121 Download
- 8 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
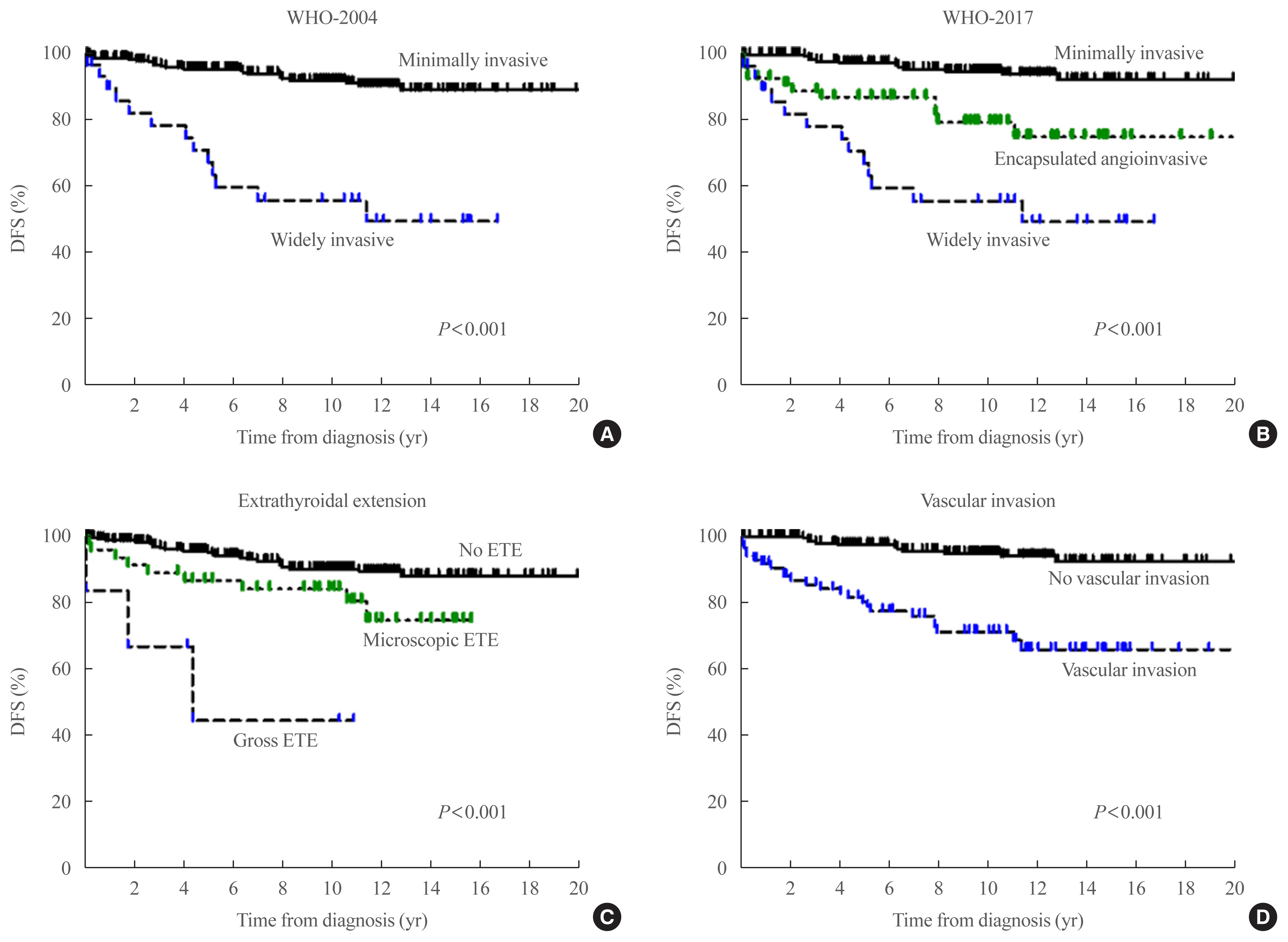
The study aimed to compare the prognostic value of the 4th edition of World Health Organization classification (WHO-2017) with the previous WHO classification (WHO-2004) for follicular thyroid carcinoma (FTC).
Methods
This multicenter retrospective cohort study included 318 patients with FTC from five tertiary centers who underwent thyroid surgery between 1996 and 2009. We evaluated the prognosis of patients with minimally invasive (MI), encapsulated angioinvasive (EA), and widely invasive (WI) FTC according to WHO-2017. Further, we evaluated the proportion of variation explained (PVE) and Harrell’s C-index to compare the predictability of disease-free survival (DFS) and disease-specific survival (DSS).
Results
In total, 227, 58, and 33 patients had MI-, EA-, and WI-FTC, respectively. During a median follow-up of 10.6 years, 46 (14.5%) patients had disease recurrence and 20 (6.3%) patients died from FTC. The 10-year DFS rates of patients with MI-, EA-, and WI-FTC were 91.1%, 78.2%, and 54.9%, respectively (P<0.001, PVE=7.1%, C-index=0.649). The corresponding 10-year DSS rates were 95.9%, 93.5%, and 73.5%, respectively (P<0.001, PVE=2.6%, C-index=0.624). The PVE and C-index values were higher using WHO-2017 than using WHO-2004 for the prediction of DFS, but not for DSS. In multivariate analysis, older age (P=0.02), gross extrathyroidal extension (ETE) (P=0.003), and distant metastasis (P<0.001) were independent risk factors for DSS.
Conclusion
WHO-2017 improves the predictability of DFS, but not DSS, in patients with FTC. Distant metastasis, gross ETE and older age (≥55 years) were independent risk factors for DSS. -
Citations
Citations to this article as recorded by- Association of Ultrasonography Features of Follicular Thyroid Carcinoma With Tumor Invasiveness and Prognosis Based on WHO Classification and TERT Promoter Mutation
Myoung Kyoung Kim, Hyunju Park, Young Lyun Oh, Jung Hee Shin, Tae Hyuk Kim, Soo Yeon Hahn
Korean Journal of Radiology.2024; 25(1): 103. CrossRef - Clinical Outcomes and Implications of Radioactive Iodine Therapy on Cancer-specific Survival in WHO Classification of FTC
Genpeng Li, Ziyang Ye, Tao Wei, Jingqiang Zhu, Zhihui Li, Jianyong Lei
The Journal of Clinical Endocrinology & Metabolism.2024;[Epub] CrossRef - Radioiodine whole body scan pitfalls in differentiated thyroid cancer
Cristina Basso, Alessandra Colapinto, Valentina Vicennati, Alessandra Gambineri, Carla Pelusi, Guido Di Dalmazi, Elisa Lodi Rizzini, Elena Tabacchi, Arber Golemi, Letizia Calderoni, Stefano Fanti, Uberto Pagotto, Andrea Repaci
Endocrine.2024;[Epub] CrossRef - The Prognostic Impact of Extent of Vascular Invasion in Follicular Thyroid Carcinoma
David Leong, Anthony J. Gill, John Turchini, Michael Waller, Roderick Clifton‐Bligh, Anthony Glover, Mark Sywak, Stan Sidhu
World Journal of Surgery.2023; 47(2): 412. CrossRef - TERT Promoter Mutation as a Prognostic Marker in Encapsulated Angioinvasive and Widely Invasive Follicular Thyroid Carcinomas
Yasuhiro Ito, Takashi Akamizu
Clinical Thyroidology.2023; 35(5): 202. CrossRef - Risk factors for death of follicular thyroid carcinoma: a systematic review and meta-analysis
Ting Zhang, Liang He, Zhihong Wang, Wenwu Dong, Wei Sun, Ping Zhang, Hao Zhang
Endocrine.2023; 82(3): 457. CrossRef - Molecular classification of follicular thyroid carcinoma based on TERT promoter mutations
Hyunju Park, Hyeong Chan Shin, Heera Yang, Jung Heo, Chang-Seok Ki, Hye Seung Kim, Jung-Han Kim, Soo Yeon Hahn, Yun Jae Chung, Sun Wook Kim, Jae Hoon Chung, Young Lyun Oh, Tae Hyuk Kim
Modern Pathology.2022; 35(2): 186. CrossRef - Whole-genome Sequencing of Follicular Thyroid Carcinomas Reveal Recurrent Mutations in MicroRNA Processing Subunit DGCR8
Johan O Paulsson, Nima Rafati, Sebastian DiLorenzo, Yi Chen, Felix Haglund, Jan Zedenius, C Christofer Juhlin
The Journal of Clinical Endocrinology & Metabolism.2021; 106(11): 3265. CrossRef - Clinicopathological Characteristics and Disease-Free Survival in Patients with Hürthle Cell Carcinoma: A Multicenter Cohort Study in South Korea
Meihua Jin, Eun Sook Kim, Bo Hyun Kim, Hee Kyung Kim, Yea Eun Kang, Min Ji Jeon, Tae Yong Kim, Ho-Cheol Kang, Won Bae Kim, Young Kee Shong, Mijin Kim, Won Gu Kim
Endocrinology and Metabolism.2021; 36(5): 1078. CrossRef
- Association of Ultrasonography Features of Follicular Thyroid Carcinoma With Tumor Invasiveness and Prognosis Based on WHO Classification and TERT Promoter Mutation

- Clinical Study
- Vandetanib for the Management of Advanced Medullary Thyroid Cancer: A Real-World Multicenter Experience
- Mijin Kim, Jee Hee Yoon, Jonghwa Ahn, Min Ji Jeon, Hee Kyung Kim, Dong Jun Lim, Ho-Cheol Kang, In Joo Kim, Young Kee Shong, Tae Yong Kim, Bo Hyun Kim
- Endocrinol Metab. 2020;35(3):587-594. Published online September 22, 2020
- DOI: https://doi.org/10.3803/EnM.2020.687

- 5,628 View
- 146 Download
- 12 Web of Science
- 12 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
Vandetanib is the most widely used tyrosine kinase inhibitor for the treatment of patients with advanced medullary thyroid cancer (MTC). However, only limited data regarding its use outside clinical trials are available. We aimed to evaluate the efficacy and safety of vandetanib in patients with advanced MTC in routine clinical practice.
Methods
In this multicenter retrospective study, 12 patients with locally advanced or metastatic MTC treated with vandetanib at four tertiary hospitals were included. The primary outcome was the objective response rate (ORR) based on the Response Evaluation Criteria in Solid Tumors. The progression-free survival (PFS), overall survival (OS), and toxicities were also evaluated.
Results
Eleven patients (92%) had distant metastasis and 10 (83%) had disease progression at enrollment. Partial response was observed in five patients (ORR, 42%) and stable disease lasting ≥24 weeks was reported in an additional five patients (83%). During the median 31.7 months of follow-up, disease progression was seen in five patients (42%); of these, two died due to disease progression. The median PFS was 25.9 months, while the median OS was not reached. All patients experienced adverse events (AEs) which were generally consistent with the known safety profile of vandetanib. Vandetanib was discontinued in two patients due to skin toxicity.
Conclusion
Consistent with the phase III trial, this study confirmed the efficacy of vandetanib for advanced MTC in terms of both ORR and PFS in the real-world setting. Vandetanib was well tolerated in the majority of patients, and there were no fatal AEs. -
Citations
Citations to this article as recorded by- Metastatic medullary thyroid carcinoma (MTC): disease course, treatment modalities and factors predisposing for drug resistance
Katerina Saltiki, George Simeakis, Olga Karapanou, Stavroula A. Paschou, Maria Alevizaki
Endocrine.2023; 80(3): 570. CrossRef - Initial Experiences of Selective RET Inhibitor Selpercatinib in Adults with Metastatic Differentiated Thyroid Carcinoma and Medullary Thyroid Carcinoma: Real-World Case Series in Korea
Han-Sang Baek, Jeonghoon Ha, Seunggyun Ha, Ja Seong Bae, Chan Kwon Jung, Dong-Jun Lim
Current Oncology.2023; 30(3): 3020. CrossRef - Molecular Basis and Natural History of Medullary Thyroid Cancer: It is (Almost) All in the RET
Nicolas Sahakian, Frédéric Castinetti, Pauline Romanet
Cancers.2023; 15(19): 4865. CrossRef - Sporadic Medullary Thyroid Carcinoma: Towards a Precision Medicine
Antonio Matrone, Carla Gambale, Alessandro Prete, Rossella Elisei
Frontiers in Endocrinology.2022;[Epub] CrossRef - Targeted therapy and drug resistance in thyroid cancer
Yujie Zhang, Zhichao Xing, Tianyou Liu, Minghai Tang, Li Mi, Jingqiang Zhu, Wenshuang Wu, Tao Wei
European Journal of Medicinal Chemistry.2022; 238: 114500. CrossRef - Daily Management of Patients on Multikinase Inhibitors’ Treatment
Carla Colombo, Simone De Leo, Matteo Trevisan, Noemi Giancola, Anna Scaltrito, Laura Fugazzola
Frontiers in Oncology.2022;[Epub] CrossRef - The Angiogenic Balance and Its Implications in Cancer and Cardiovascular Diseases: An Overview
Cătălina Ionescu, Bogdan Oprea, Georgeta Ciobanu, Milena Georgescu, Ramona Bică, Garofiţa-Olivia Mateescu, Fidan Huseynova, Veronique Barragan-Montero
Medicina.2022; 58(7): 903. CrossRef - Reassessing vascular endothelial growth factor (VEGF) in anti-angiogenic cancer therapy
Tobiloba C. Elebiyo, Damilare Rotimi, Ikponmwosa O. Evbuomwan, Rotdelmwa Filibus Maimako, Matthew Iyobhebhe, Oluwafemi Adeleke Ojo, Olarewaju M. Oluba, Oluyomi S. Adeyemi
Cancer Treatment and Research Communications.2022; 32: 100620. CrossRef - Current Guidelines for Management of Medullary Thyroid Carcinoma
Mijin Kim, Bo Hyun Kim
Endocrinology and Metabolism.2021; 36(3): 514. CrossRef - Recent advances in precision medicine for the treatment of medullary thyroid cancer
Jolanta Krajewska, Aleksandra Kukulska, Malgorzata Oczko-Wojciechowska, Barbara Jarzab
Expert Review of Precision Medicine and Drug Development.2021; 6(5): 307. CrossRef - Functional evaluation of vandetanib metabolism by CYP3A4 variants and potential drug interactions in vitro
Mingming Han, Xiaodan Zhang, Zhize Ye, Jing Wang, Jianchang Qian, Guoxin Hu, Jianping Cai
Chemico-Biological Interactions.2021; 350: 109700. CrossRef - Nephrotoxicity in advanced thyroid cancer treated with tyrosine kinase inhibitors: An update
Alice Nervo, Francesca Retta, Alberto Ragni, Alessandro Piovesan, Alberto Mella, Luigi Biancone, Marco Manganaro, Marco Gallo, Emanuela Arvat
Critical Reviews in Oncology/Hematology.2021; 168: 103533. CrossRef
- Metastatic medullary thyroid carcinoma (MTC): disease course, treatment modalities and factors predisposing for drug resistance

- Thyroid
- Association between Serum Free Thyroxine and Anemia in Euthyroid Adults: A Nationwide Study (Endocrinol Metab 2020;35:106-14, Mijin Kim et al.)
- Mijin Kim, Bo Hyun Kim
- Endocrinol Metab. 2020;35(3):669-670. Published online July 30, 2020
- DOI: https://doi.org/10.3803/EnM.2020.306
- 4,087 View
- 72 Download

- Clinical Study
- Modification of the Tumor-Node-Metastasis Staging System for Differentiated Thyroid Carcinoma by Considering Extra-Thyroidal Extension and Lateral Cervical Lymph Node Metastasis
- Mijin Kim, Won Gu Kim, Min Ji Jeon, Hee Kyung Kim, Hyon-Seung Yi, Eun Sook Kim, Bo Hyun Kim, Won Bae Kim, Young Kee Shong, Ho-Cheol Kang, Tae Yong Kim
- Endocrinol Metab. 2020;35(1):149-156. Published online March 19, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.1.149
- 5,244 View
- 82 Download
- 6 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
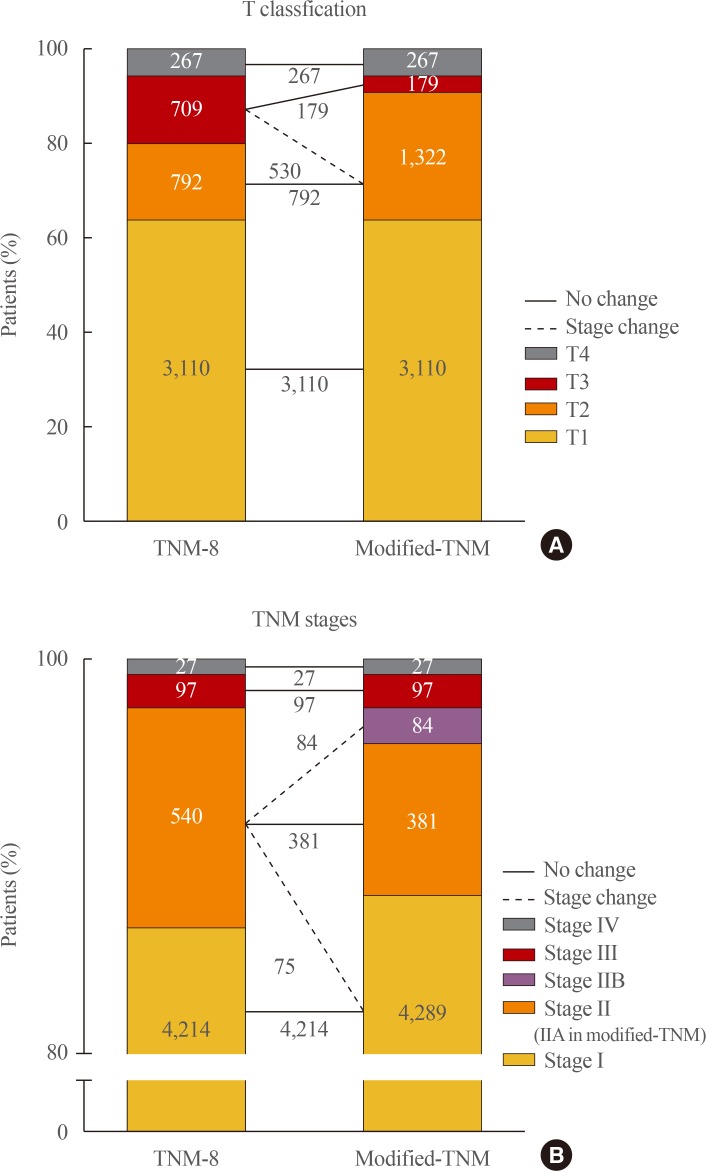
ePub Background Concerns have arisen about the classification of extra-thyroidal extension (ETE) and lateral cervical lymph node metastasis (N1b) in the 8th edition of the tumor-node-metastasis staging system (TNM-8). This study evaluated the prognostic validity of a modified-TNM staging system, focusing on ETE and N1b, in differentiated thyroid carcinoma (DTC) patients.
Methods This multicenter retrospective cohort study included 4,878 DTC patients from five tertiary hospitals. In the modified-TNM, T3b in TNM-8 was down-staged to T2, and stage II was subdivided into stages IIA and IIB. Older patients with N1b were reclassified as stage IIB.
Results The modified-TNM resulted in staging migration in 540 patients (11%) classified as stage II according to the TNM-8, with 75 (14%), 381 (71%), and 84 patients (16%) classified as stages I, IIA, and IIB, respectively. The 10-year disease-specific survival (DSS) rates in patients classified as stages I, II, III, and IV by TNM-8 were 99.8%, 95.9%, 81.0%, and 41.6%, respectively. The DSS rates of patients classified as stages I, IIA, IIB, III, and IV according to the modified-TNM were 99.8%, 96.4%, 93.3%, 81.0%, and 41.6%, respectively. DSS curves between stages on TNM-8 (
P <0.001) and modified-TNM (P <0.001) differed significantly, but the modified-TNM discriminated better than TNM-8. The proportions of variation explained values of TNM-8 and modified-TNM were 6.3% and 6.5%, respectively.Conclusion Modification of the TNM staging system focusing on ETE and N1b could improve the prediction of DSS in patients with DTC. Further researches are needed to validate the prognostic accuracy of this modified-TNM staging system.
-
Citations
Citations to this article as recorded by- Clinicopathological features of differentiated thyroid carcinoma as predictors of the effects of radioactive iodine therapy
Wen Liu, Beibei Jiang, Jingli Xue, Ruijing Liu, Yuqing Wei, Peifeng Li
Annals of Diagnostic Pathology.2024; 69: 152243. CrossRef - Thyroid Collision Tumors: The Presence of the Medullary Thyroid Carcinoma Component Negatively Influences the Prognosis
Ion Negura, Victor Ianole, Mihai Danciu, Cristina Preda, Diana Gabriela Iosep, Radu Dănilă, Alexandru Grigorovici, Delia Gabriela Ciobanu Apostol
Diagnostics.2023; 13(2): 285. CrossRef - Serum thyroglobulin testing after thyroid lobectomy in patients with 1–4 cm papillary thyroid carcinoma
Ahreum Jang, Meihua Jin, Chae A Kim, Min Ji Jeon, Yu-Mi Lee, Tae-Yon Sung, Tae Yong Kim, Won Bae Kim, Young Kee Shong, Won Gu Kim
Endocrine.2023; 81(2): 290. CrossRef - Prognostic Impact of Microscopic Extra-Thyroidal Extension (mETE) on Disease Free Survival in Patients with Papillary Thyroid Carcinoma (PTC)
Nadia Bouzehouane, Pascal Roy, Myriam Decaussin-Petrucci, Mireille Bertholon-Grégoire, Chantal Bully, Agnès Perrin, Helene Lasolle, Jean-Christophe Lifante, Françoise Borson-Chazot, Claire Bournaud
Cancers.2022; 14(11): 2591. CrossRef - Impacts of the American Joint Committee on Cancer (AJCC) 8th edition tumor, node, metastasis (TNM) staging system on outcomes of differentiated thyroid cancer in Thai patients
Yotsapon Thewjitcharoen, Waralee Chatchomchuan, Krittadhee Karndumri, Sriurai Porramatikul, Sirinate Krittiyawong, Ekgaluck Wanothayaroj, Siriwan Butadej, Soontaree Nakasatien, Veekij Veerasomboonsin, Auchai Kanchanapituk, Rajata Rajatanavin, Thep Himatho
Heliyon.2021; 7(3): e06624. CrossRef
- Clinicopathological features of differentiated thyroid carcinoma as predictors of the effects of radioactive iodine therapy


 KES
KES

 First
First Prev
Prev



